You’re probably reading this because at some point in your life you’ve had shoulder pain, or maybe because you have shoulder pain now that hasn’t gotten better.
Shoulder pain is very common among adults of all ages. Persistent shoulder pain can result from bursitis, tendinitis, rotator cuff tear, adhesive capsulitis (frozen shoulder), impingement syndrome, avascular necrosis, osteoarthritis (OA), other causes of degenerative joint disease or from a current or past traumatic injury.
The rotator cuff of the shoulder is made up of four muscles. Tendons of these muscles come together to form a cuff around the head of the upper arm bone (humerus) and top of the shoulder. The rotator cuff muscles are important stabilizers and movers of the shoulder joint. As the name implies, the rotator cuff functions to allow you to rotate your shoulder and lift your arm.
Some shoulder conditions may have complex causes, but they can usually be diagnosed on the basis of medical history, a physical examination consisting of special tests including range of motion and strength tests. Although a $3,000 MRI may confirm that you have a partial tear, it is not always necessary as it will not change the outcome.
Rotator cuff tendonitis is the inflammation of the rotator cuff tendons and muscles that help move your shoulder joint. This injury typically occurs over time, usually as a result of keeping your shoulder in a single position for a prolonged period (such as sleeping on your shoulder every night or keeping your hand under your head), by doing repeated overhead work-related activities, or repetitive athletic activities such as basketball, baseball, wrestling, tennis, etc.
A rotator cuff tear can be either partial or complete. A partial tear is when one of the tendons of the rotator cuff is frayed or damaged. A complete tear (also called a full-thickness tear) is when the tendon is severed in half or pulled completely off of the bone. Rotator cuff tears can occur over time from repeated wear and tear or as an acute traumatic injury such as a fall on the arm/shoulder, heavy lifting, car accidents, starting a lawnmower, or sudden reaching behind to grab something from the back seat.
Another common cause of shoulder pain that is often missed is that your shoulder pain may be coming from your neck. If that’s the case, your shoulder x-ray and MRI would look normal which can lead to more frustration, especially when a medical provider tells you that there is nothing wrong.
Physical therapy is a clinically proven conservative method of treating shoulder and neck issues. Multiple studies validate the effectiveness of PT for shoulder pain and how it can prevent unnecessary surgeries. A good physical therapist should be focused on treating the root cause of the pain rather than just treating the symptoms.
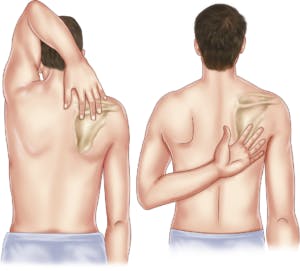
Experiencing shoulder pain? Try doing the exercise in the picture below:
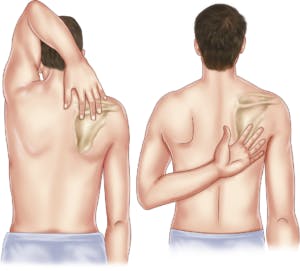
- Take the arm on the affected side and reach over your head and behind your neck to touch your shoulder blade on the opposite side.
- Next, take the arm on the affected side and reach below your neck and behind your back to touch your shoulder blade.
If you are not able to reach all the way or if the pain is preventing you from doing so, it is indicative of possible rotator cuff injury.
Now try moving your shoulders up, sideways, and try bending your neck down… if the pain in your shoulder increases, it’s possible that your neck may be the cause of your pain.
Either way, pain is the body’s way of telling you that something is wrong. I often find
people trying to diagnose their pain by using google, which can often lead to people making mistakes that may make their pain worse. The biggest mistake people make is to ignore the pain or to alter it by taking pain killers, narcotics, or steroid injections. By seeing a specialty-trained physical therapist right away, you may prevent costly surgeries, worsened injuries, or permanent damage to your shoulders.